Early Intervention in Peri-Implant Disease – Insights from the 2024 AO/AAP Consensus
The recently published Academy of Osseointegration/American Academy of Periodontology (AO/AAP) Consensus Report emphasizes a clear message: peri-implant mucositis is reversible—peri-implantitis often is not. The consensus underscores that the key to preserving implants is early identification and treatment of mucositis before it progresses to peri-implantitis, which involves loss of supporting bone and carries a faster, more aggressive destruction rate than periodontitis. Risk factors for disease initiation and progression include a history of periodontitis, smoking, uncontrolled diabetes, obesity, excess alcohol intake, and local factors such as inadequate keratinized mucosa, implant malpositioning, and unfavorable prosthetic design.
Evidence-based treatment recommendations reaffirm that mechanical debridement is the cornerstone therapy for peri-implant mucositis, with adjunctive measures offering limited additional benefit in most cases. Regular supportive peri-implant maintenance—typically every 3 to 4 months for higher-risk patients—is critical to long-term success. Once peri-implantitis has developed, more invasive and less predictable surgical interventions (either nonreconstructive or reconstructive) are often necessary, but complete resolution is more challenging to achieve.
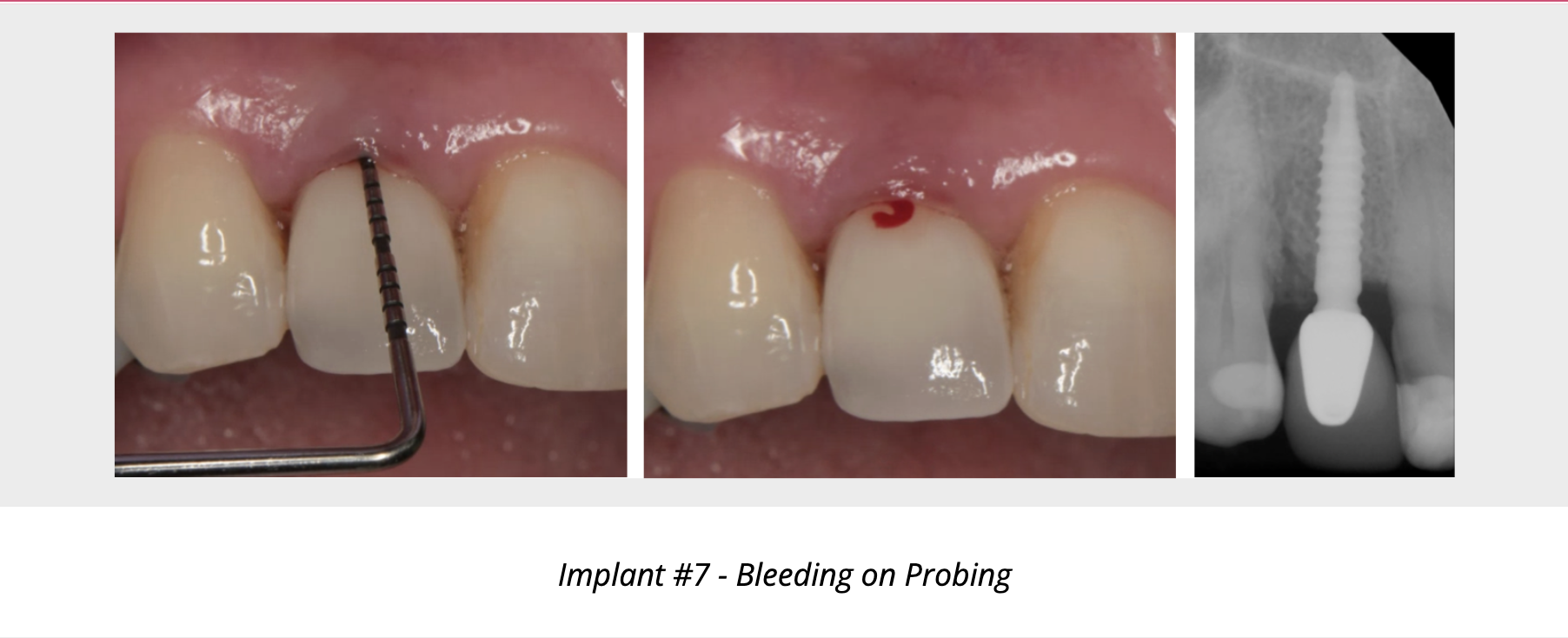
Prompt treatment at the first clinical signs of peri-implant mucositis—bleeding on probing, erythema, swelling, or suppuration —can prevent complex and costly peri-implantitis treatment down the road. Early collaboration allows us to address reversible inflammation, optimize risk factors, and implement individualized maintenance protocols, helping to protect your patients’ implants and long-term oral health.